
Wondering how much do we really get fmo PhilHealth in cases we get sick? Then read on.
From fee for service, that is computing every single item of your expense. Right now, PhilHealth is now paying it at a package called “All Case Rates Provider Payment Scheme.”
With the successful implementation of the first 23 medical and surgical conditions under the case rate system in September 2011, PhilHealth endeavored to implement case rates. This time, for all cases and conditions.
Case rate means a fixed-rate or amount will be reimbursed by PhilHealth for a specific illness or case. Prior to this shift, PhilHealth has applied the Fee-For-Service or FFS payment scheme were in health care providers are paid for each service they provide.
No Balance Billing
No Balance Billing is a program that allows every member access to healthcare from public hospitals without paying more than the required case rates.
This means if you used public hospital for a certain disease included in the PhilHealth Case Rate. You should not be paying more than the required case rates given by the PhilHealth. Paying more than the fixed case rates usually happens if you use other institution other than the public hospitals.
Inpatient Benefits (Confined in the Hospital)
Availment condition: Member must have at least three (3) months’ premium contributions within the immediate six (6) months prior to the month of availment.
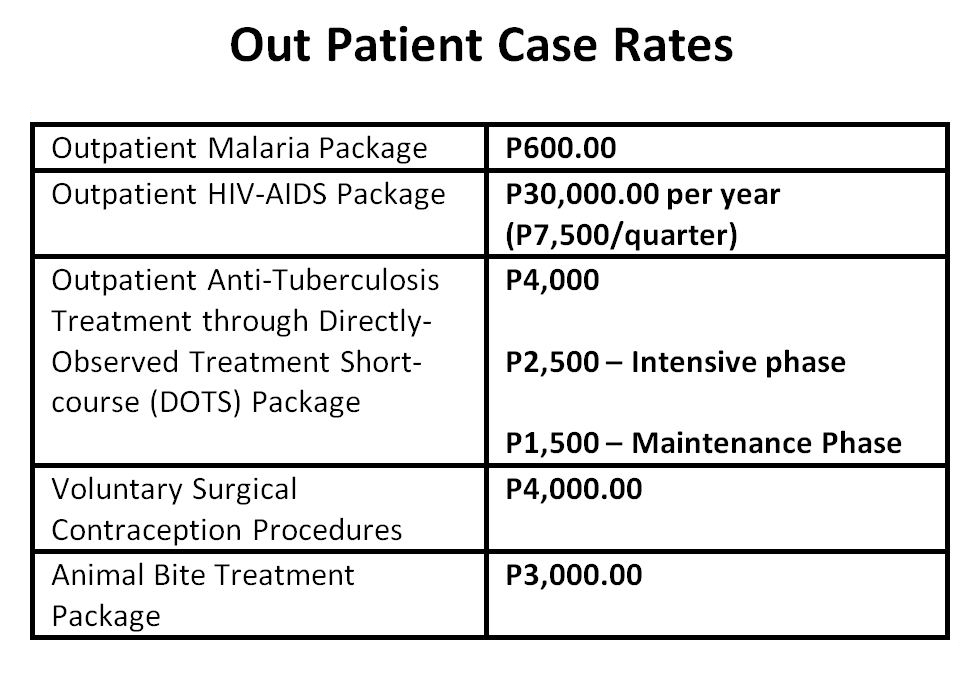
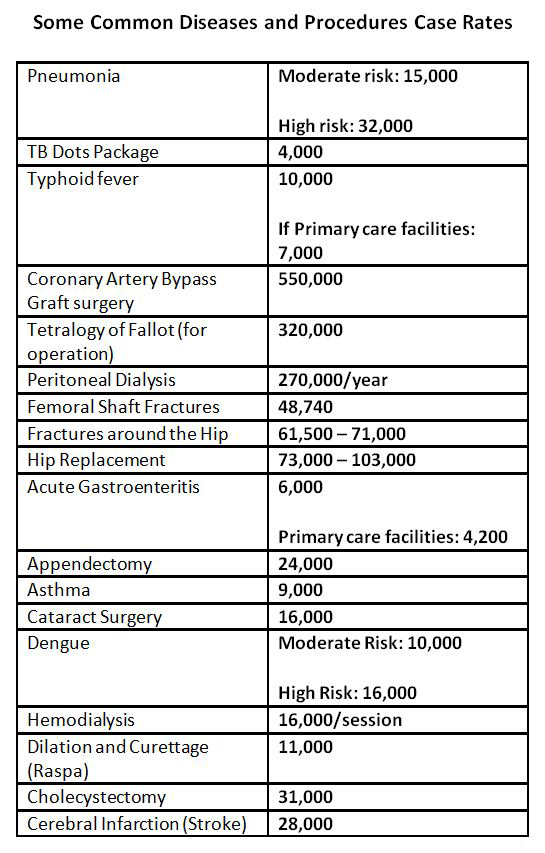
Some Common Diseases and its Fixed Case Rates:
Case Rates Coverage:

As you can see, PhilHealth cannot be the only answer to the health problem all Filipinos face. You have to be more ready if the time comes you get diagnosed with a more money draining illness. Make sure you have a personal plan that can get you through your disease. Take charge of your own health.
Read this:
The Importance of Critical Illness plan in Holistic Financial Planning
“Money can pay fees at the hospital but can’t buy you health.”
Please be guided accordingly.

For other diseases and case rates, do visit: www.philhealth.gov.ph
Watch out on the next part of this series. The Critical illness package of PhilHealth.
Read More:
- Dissecting PhilHealth: Know your Rights and Benefits Part 1
- Dissecting Pag-IBIG Fund: What is there to Love?
- Hurdles of Financial Freedom Mga Balakid sa inyong Pagyaman)
- Make Sure you have Critical Illness rider in your Life Insurance Policy
Latest posts by Pinky De Leon-Intal, MD, RFC (see all)
- Say Goodbye to Chronic Lifestyle Diseases (Hypertension, Diabetes, Cancer, Gout, etc.) with Right Food and Right Water - 23 May, 2023
- Embracing Superpowers: A Mom’s Journey as a Doctor, Professor, and Financial Consultant - 19 May, 2023
- Celebrating the Power of Women: Honored by Philippine Daily Inquirer - 17 May, 2023


I use PHILHEALTH for my chemo treatments. How much can I max out of it frOM PHILHEALTH?
I saw this:
Rules on Chemotherapy Coverage:
Chemotherapy (RVS 96408)
a. The case rate amount for chemotherapy is equivalent to one cycle of chemotherapy.
b. One cycle of chemotherapy is equivalent to 2 days deduction from the 45 days benefit allowance.
c. Chemotherapy may be claimed as inpatient or outpatient.
i. If claimed as inpatient and in the same hospital, the chemotherapy package may be claimed as first or second case rate.
ii. Multiple cycles may be claimed in one claim form for both inpatient and outpatient chemotherapy. The dates of each cycle claimed shall be indicated in the space provided in Claim Form 2.
Source: Philhealth Circular No. 0035 s. 2013 — ACR Policy No. 2 — Implementing Guidelines on Medical and Procedure Case Rates